Bone loss is very common, especially in older people, and for many people, adding exercise and bone-healthy nutrition from food and/or supplements can help or cure the problem.
However, in addition to diet and exercise, you should find out if you have any medical issues that can interfere with your body’s bone-making process. If you do, the nutritional and exercise advice provided here can certainly help, but you might not be able to achieve normal or near normal bone density.
Ask your doctor to order the following tests to pinpoint medical issues that interfere with the bone making process:
1. Urine test for calcium: Calcium Urine, Timed to find out if you are getting enough calcium. When your body needs calcium and you are not getting enough in your diet or by supplementation, it takes the calcium from your bones and puts it into your blood. A normal or great blood test for calcium levels can be covering up that you are not getting enough calcium to maintain healthy bones.
2. Parathyroid gland test: The parathyroid gland keeps your calcium levels balanced. If the parathyroid hormone becomes imbalanced, your bones can become weak and porous, which results in low bone density.
3. Calcitonin test: Your body makes the calcitonin hormone in the thyroid gland. It’s role is to help regulate calcium levels in your blood by increasing and decreasing the calcium levels to manage the bone remodeling process.
Additional tests can include CBC (complete blood cell) and vitamin D3 levels.
Proton Pump Inhibitors
Proton pump inhibitors (PPIs), can interfere with the bone remodeling process too and result in low bone density and increased fracture risk. If you want to know more, read:
“Healing Heartburn Naturally – A Guide to Managing Acid Reflux and Restoring Gut Health” by Dr. Tieraona Low Dog, MD.
Her book offers a lot of information on how to safely taper off acid-suppressing medications and strategies for optimizing health after long-term PPI use. She also covers how to stay healthy while takking PPIs if long-term PPI use is necessary.
Our body’s bone remodeling process is very involved. In my opinion, I think that is why bone drugs that target a particular aspect of the bone making process don’t work very well for most people and have so many possible side effects.
Your body knows exactly what to do with nutrients like calcium, magnesium, and D3, but drugs are foreign substances. They can do some good, but typically only help a little and can have bad side effects. You also have to stop taking them or change to another drug after a few years.
I think the natural approach is worth trying, and should be tried with weight-bearing exercise before you resort to drugs. Even if it doesn’t help your bones because you have a problem in your thyroid or parathyroid glands, the natural approach will, at the very least, leave you in better bone health and better overall health.
This is why I think the natural approach is worth trying, and should be tried before resorting to drugs. Even if it doesn’t help your bones because you have a problem in your thyroid or parathyroid glands, the natural approach will, at the very least, leave you in better health. The natural approach has no side effects (except maybe if you have food allergies), and if you make it a lifestyle change, then any improvement you get could last your lifetime.
Nature vs. Bone Drugs
One thing I have learned in my journey from diseased to healthy bones is that our body’s bone remodeling process is very intricate. In my personal opinion, I think that is why bone drugs that target a particular aspect of the bone making process don’t work very well and have so many side effects.
Your body knows exactly what to do with nutrients like calcium, magnesium, and D3, but drugs are foreign substances. They can do some good, but they might only help a little and can have unwanted side effects. You also have to stop taking them or change to another drug after a few years.
This is why I think the natural approach works much better, and should be tried with weight bearing exercise before you resort to drugs. Even if it doesn’t help your bones because you have a problem in your thyroid or parathyroid glands, the natural approach will at the very least leave you in better health. The natural approach has no side effects (except maybe if you have food allergies), and if you make it a lifestyle change, then the improvement will likely last for your lifetime.
If you want to be really, really thorough with testing, here is a very comprehensive list of tests for assessing bone health put together by Dr. Keith McCormick, Chiropractor:
*
Keep reading for detailed information bone nutrition and weight bearing exercise options. There are all important if you want to build and maintain strong, healthy, non-osteoporotic bones without bone drugs.
In this document
Nutrients for Bone Building
Estrogen
Chinese Herbs for Menopause Support
Exercise
Yoga
Qi Gong and Tai Chi
Yoga Sequences for Bone Health
The following sections walk through everything that I know that you can do to improve your bone density short of taking bone drugs.
Nutrients for Bone Building
While a lot of people might think they need more or better weight-bearing exercise if they have low bone density, that isn’t always the case.
Exercising, no matter how much, won’t help you build bone density if your body either 1) doesn’t have the right nutrients to do the job, or 2) has something wrong in the thyroid or parathyroid glands that would inhibit the bone remodeling process. See my first post for more information about testing the parathyroid and thyroid gland. As far as nutrients go, it doesn’t matter to your body if you take supplements, or get the nutrients from your food, or a combination.
Bone remodeling is the continuous process by which your body removes old bone tissue from and adds new bone tissue to your skeleton. The bone remodeling process requires that specific nutrients be available in your body to help maintain a balanced activity of bone remodeling. If there is a lack of any of these nutrients or some other imbalance in the bone remodeling cycle, the strength, flexibility, and integrity of your bones will degrade over time.
Bone tissue is about 70% mineral content and 30% organic matter:
- Mineral portion: 95% is calcium hydroxyapatite, and the rest is sodium, magnesium, fluoride, and strontium. Hydroxyapatite is a calcium and phosphorus compound found in teeth and bone.
- Organic portion: 98% is collagen fibers, and the remaining 2% is a supporting matrix of glycoproteins and proteoglycans.
I recommend the forces that yoga generates – doing Series I every day at least once – and 40+ grams of protein, 1500 mg. of calcium, 1500 IU of vitamin D3, 250 – 400 mg of magnesium and 90 mcg of vitamin K2, all daily. Please don’t overdo the protein, too much can harm the kidneys, but 50 – 175 grams a day will stand you in good stead with a 2000 calorie diet.
– Dr. Fishman from his newsletter.
Calcium
Besides being the primary mineral in your bones, calcium is also important for muscle contraction, nerve conduction, and intracellular signaling.
Calcium metabolism has a direct influence on whether your body removes old bone from your body and adds new bone. This bone remodeling process is regulated by the interplay between parathyroid hormone (PTH), which stimulates bone resorption; and calcitonin, a hormone that reduces calcium in the blood. Also, factors such as genetics, hormones, physical activity, and nutrition, influence whether your body removes old bone and adds new bone. A drop in the calcium level in your blood triggers the removal of old bone, which can result in a decline of bone-mineral density if your body does not make enough new bone.
The recommended total intake of calcium (diet plus supplementation) for adults is 1,000 to 1,400 mg per day. Dietary calcium sources include the following:
- Dairy products such as milk, cheese, yogurt, and so on.
- Vegetables in the Brassica family (broccoli, kale, cabbage).
- Dark-green leafy vegetables (collards, dandelion greens, beet greens).
- Some nuts and seeds.
- Canned fish with bones.
- Calcium in mineral water has been shown to support healthy bone-mineral density in some studies.
- Dark chocolate
Sometimes calcium supplementation is necessary because you are not getting enough calcium from your diet. Your blood calcium levels might be fine, but this might mean that your body is getting calcium from your bones and storing it in your blood to supplement the deficit. If you have osteoporosis or osteopenia, it is a good idea to have your doctor order a 24 hour urine test for calcium. If you are not getting enough calcium from your diet and/or supplementation, it will become apparent from this test, regardless of what your blood levels are.
Many, if not most, persons fall short of the 1200-1500 mg recommendation for people over age 50. The recommendation might be due to a concern about calcification of soft tissues. However, calcification of soft tissues is not necessarily due to calcium intake, but to a lack of magnesium and vitamin K2.
The two most common supplement forms are calcium carbonate and calcium citrate.
- Calcium carbonate requires stomach acid to be absorbed so people with low stomach acid should take a different kind of calcium.
- Calcium citrate does not require stomach acid to be absorbed. Some people say that calcium citrate is more absorbable than calcium carbonate, but this might not be true. A randomized trial of 24 postmenopausal women found that calcium carbonate and calcium citrate produced equivalent increases in blood serum calcium levels over 24 hours.
Chelated forms of calcium such as Calcium lysinate might have superior bioavailability. Calcium lysinate showed superior bioavailability compared to both calcium carbonate and calcium citrate in a clinical trial.
Calcium microcrystalline hydroxyapatite (MCH) is extracted from animal bone. A randomized trial with 100 postmenopausal women found that MCH increased blood levels of calcium at a lower rate than either calcium citrate or calcium carbonate, but had an equivalent effect on bone turnover. Now there is a manufactured form of MCH called nano hydroxiapatite, which is vegan. There is already a toothpaste with nano hydroxyapetite. I think calcium supplements will soon follow if they have not already.
Note: When you consume calcium (through food, supplementation, or both), the amount absorbed into the body decreases as the intake increases. It is best to spread calcium intake, especially in supplemental form, over the day and to consume no more than 500 mg at a time.
If you are looking for a high-quality calcium supplement see Jarrow Formulas.
Protein
You should get at least 1 gram of protein per kilogram of body weight. One kilogram = 2.2 lbs. The following quote is from https://www.healthline.com/health/total-protein.
Protein makes up ~50% of bone volume and approximately one-third of its mass. It provides the structural matrix of bone, whereas calcium is the dominant mineral within that matrix. Collagen and a variety of noncollagenous proteins form the organic matrix of bone, so an adequate dietary protein intake would seem to be essential for optimal acquisition and maintenance of adult bone mass. Considerable attention has recently also focused on dietary protein’s role in the mature skeleton, prompted in part by an increasing interest in nonpharmacological approaches to maintaining skeletal health in adult life and later adult years.
Vitamin D3
Vitamin D3 has an important role in many physiologic functions such as muscle strength, immunity, inflammation, mood, and bone health. In bone health, vitamin D3 promotes the absorption of calcium from the gastrointestinal tract. Studies have suggested that:
- Vitamin D3 and calcium confer the most benefit to bones when consumed together.
- Without adequate vitamin D3 levels, only 10 to 15 percent of dietary calcium is absorbed.
- When a person’s vitamin D3 stores are adequate, calcium absorption increases by 30 to 40 percent.
Dr. Dale Bredesen, an expert and pioneer on brain health, recommends a blood serum level of Vitamin D3 in the range of 50-80 ng/mL. This level is likely also good for your bones.
Magnesium and Vitamin D3
Magnesium is stored in bones, skeletal muscle, and soft tissues. In bones, magnesium is incorporated in the hydroxyapatite portion of the bone tissue where it contributes to bone tissue structure. Magnesium is also required for your body to make calcitonin–a hormone that reduces calcium in the blood and thereby inhibits bone breakdown.This process is explained further in Bone Remodeling and Bone Drugs.
In addition, magnesium promotes alkaline phosphatase activity (a critical enzyme for bone formation), vitamin D3 metabolism and activation to enhance calcium absorption in the GI tract. Magnesium also enables vitamin D3 to bind to its own transport protein to reach and be activated in the liver. Sources of dietary magnesium:
However, the U.S. National Health and Nutrition Examination Surveys show that most Americans consume less than the recommended intake of magnesium (310 to 420 mcg per day for adults). Consequently, magnesium supplementation might be necessary.
Most people who take supplemental calcium should also take supplemental magnesium. The recommended ratio of calcium to magnesium intake is about 2:1. You might want to consider your dietary intake of calcium and magnesium before deciding how much of each to supplement.
Some studies have found that magnesium in forms of aspartate, citrate, lactate, or chloride are absorbed more readily and are more bioavailable than magnesium oxide or magnesium sulfate. A small comparison study between chelated magnesium (magnesium bisglycinate) and magnesium citrate showed that magnesium citrate had better bioavailability than magnesium bisglycinate. However, magnesium glycinate is less likely to have bowel effects and might be tolerated better for some people than other forms.
Phosphorus
Calcium needs phosphorus to maximize its own strengthening benefits for strong bones and teeth. The daily recommended dose is 700 mg/day, and it is found in many foods. Side effects if you do not get enough include anxiety, loss of appetite, grumpiness, mood changes, trouble breathing, and sluggishness.
Example food sources of phosphorus:
- Pork
- Chicken
- Organic meats
- Fish
- Cheddar cheese
- Nutty spread
- Corn
- Broccoli
- Sunflower and Pumpkin Seeds
- Quinoa
- Amaranth
- Whole wheat
- Beans and Lentils
- Soy
- Garlic
- Nuts
- Dark chocolate
Vitamins K1 and K2
Vitamin K is a group of fat-soluble vitamins with similar chemical structures. The two forms common in the human diet are vitamins K1 and K2. Both forms are important for blood clotting and bone health.
Vitamin K1 is mostly found in plant foods like green leafy vegetables and is about 75% to 90% of all vitamin K consumed by humans. Vitamin K2 is found in fermented foods, animal products, and is produced by gut bacteria. K2 has some subtypes called menaquinones (MKs). Their name is related to the length of their side chain, and range from MK-4 to MK13. The two main forms are MK-4 and MK-7.
- MK-4 stays in the body for about 8 hours. It is found in pasteurized eggs, meats, and dairy, and has been shown to reduce fractures, but does not have the same circulatory benefits as MK-7.
- MK-7 stays in the body for 24 hours or more. It is found in some fermented food, but is harder to find in the western diet. MK-7 has been shown to reduce bone loss, enhance bone formation, and reduce arterial stiffness by directing calcium to the bones and removing arterial plaque.
Vitamins K (K1 and K2) with D3 play a critical role in how your body deposits calcium into new bone. Bone building takes place after a series of chemical processes that result in carboxylated osteocalcin binding to calcium to build bone by depositing calcium into the hydroxyapatite of the bone. Carboxylated osteocalcin is essential for bone mineralization.
The Institute of Medicine has established no upper limit for vitamin K, stating that consumption of the vitamin is unlikely to cause adverse health effects.
MK-4 at 45 mg/day is a standard practice in Japan to support women’s bone health after menopause. Proponents of MK-4 cite studies conducted in Japan and other Asian countries that demonstrate benefits for bone health. In 2019, researchers compared daily MK-4 intakes of 5 mgs and 45 mgs. 5 mgs of MK-4 per day positively affected carboxylated osteocalcin levels, but 45 mgs offered no additional benefit.
MK-7 is widely available in dietary supplements in the United States. Recommended intakes are much lower than 45 mg per day. Although, it is usually taken between 45 mcg and 90 mcg per day, studies have evaluated intakes of up to 200 mcg per day as safe.
Probiotics and Bone Health
There are up to 1,000 species of bacteria in your gut microbiome that not only influence gastrointestinal and immune health, but are also involved in a number of mechanisms that affect bone health. A strong microbiome provides the following benefits to bone health:
Proven to reduce inflammation. The result of reduced inflammation is a strong digestive system where you get the maximum nutrition from the food you eat, which frees up more calcium, magnesium, vitamin K, D3, and other important bone minerals. Your body has the nutrients it needs to make strong, dense bones.
Increased synthesis of gut vitamins. Your gut uses probiotic bacteria to produce vitamins such as D, C, K, and folate. These vitamins are essential for managing the calcium in your body for forming bone.
Regulate your parathyroid hormone (PTH) levels. When your PTH levels go up, osteoclasts (see Bone Remodeling and Bone Drugs.) activate and break down bone. This process releases calcium into your blood and is intended to keep your blood calcium levels steady. Probiotics help maintain your PTH at steady levels, and this keeps osteoclast activity balanced. Balanced osteoclast activity helps your body maintain healthy calcium levels in your bones.
Best probiotics for osteoporosis:
- L. Helveticus
- L. salivarius
- L. reuteri
- B. Longum
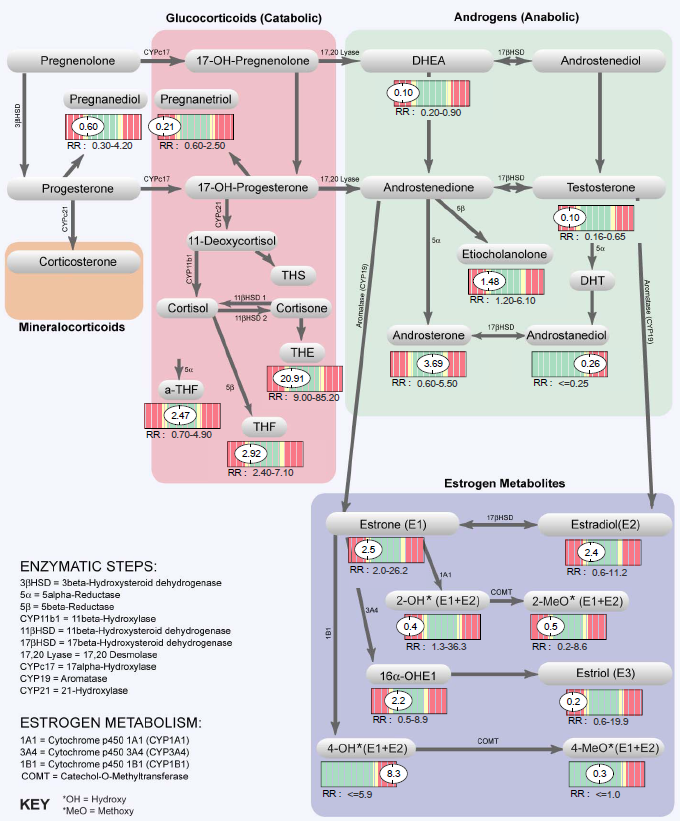
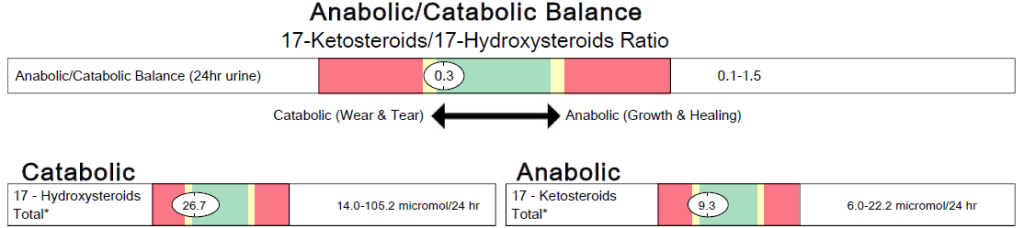
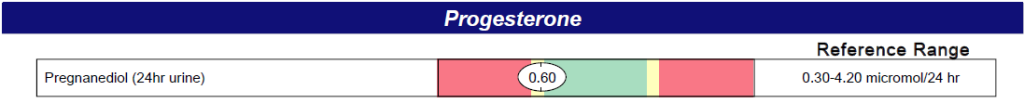
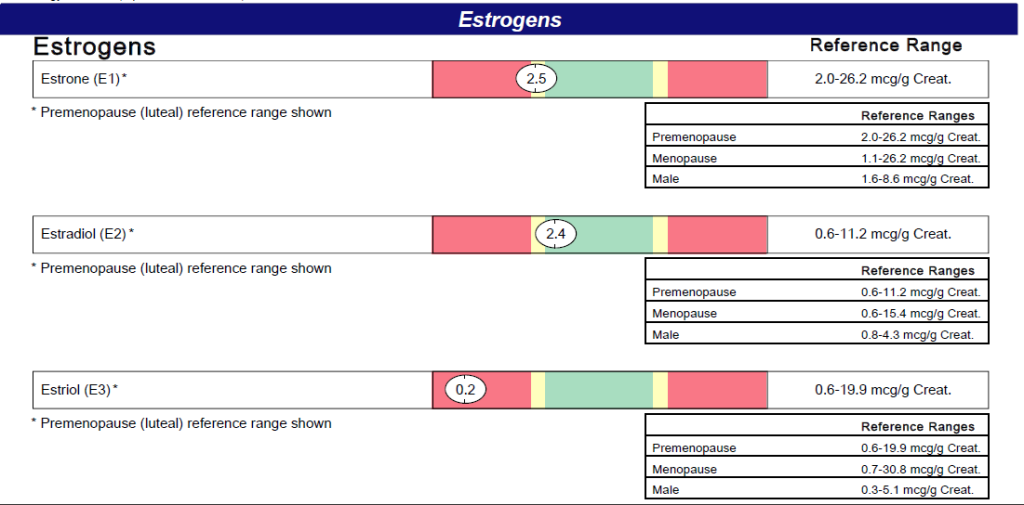
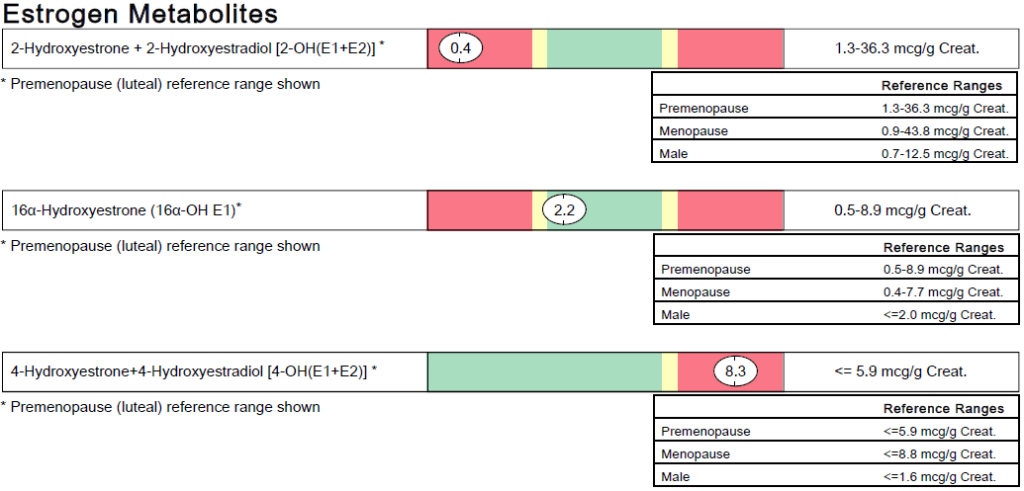
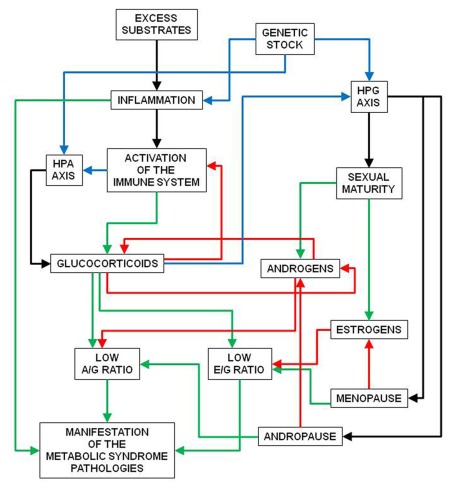
Estrogen
Estrogen is a category of sex hormones that keeps cholesterol under control, protects bone health in women and men, and affects the brain, mood, heart, skin, and other tissues. Studies have found that estrogens play an important role in the regulation of bone mass and bone strength in humans by managing the activities of bone-forming osteoblasts and bone-reabsorbing osteoclasts. Not enough estrogen can cause the balance between bone formation and bone resorption to tip in favor of resorption. Over time this results in bone loss due to too much bone resorption.
A woman’s body produces the following 3 types of estrogen, each with a distinct function in the body:
- Estradiol (E2). The most common estrogen in women of childbearing age, and used in hormone replacement therapy (HRT) for post-menopausal women. It is the most potent estrogen of the three. Its main function in a woman’s body is to mature and maintain the reproductive system.
- Estriol (E3). The main estrogen during pregnancy. It is much less potent than estradiol. It promotes uterine growth and prepares a woman’s body for giving birth.
- Estrone (E1). The only estrogen your body makes after menopause. It is much less potent than either estradiol or estrone. A woman’s body can metabolize estrone into estradiol.
Dr. Fishman provides detailed information about the complex effects of hormones in the human body in his book, Yoga for Osteoporosis.
Estrogen Receptors
Estrogen receptors are a group of proteins found inside cells that are activated by estrogen. Estrogen receptors are distributed throughout the body in the uterus, vagina, breast, pelvis, skin, bladder, urethra, bones, and brain, and play an important role in the overall health of these organs.
If your body is not producing enough estrogen, the receptors deactivate. However, if you start hormone replacement therapy (HRT), even if it is many years after your body stopped making estrogen, the receptors will slowly wake up to normal or nearly normal and resume their various roles.
Prescription HRT
When hormone replacement therapy is prescribed by a doctor for post-menopausal symptoms, the options are transdermal or oral. Transdermal administration can be patches, gels, or creams. Oral administration is a once-a-day pill. Either way, the estrogen can be derived from bioidentical estrogens or equine conjugated estrogens.
- Bioidentical estrogens are chemically identical to the estrogen made by your body and come from plants such as soy, yams, sunflower seeds, poppy seeds, and other plants.
- Conjugated equine estrogens are a mixture of the sodium salts of estrogen conjugates found in horses. They are available as preparations manufactured from pregnant mare urine, or as synthetic replications of the natural preparations.
- Skin patches are administered at much lower doses than tablets. In most cases the tablets are 0.625 to 1 mg once a day. In contrast, the skin patches come in .025mg, .05mg, .075 mg, and .1 mg administered throughout the day.
- A doctor typically orders estradiol blood level tests over a period time to determine the estradiol blood levels to figure out which patch or tablet strength produces the optimum estradiol blood level for a given person. An estradiol range of 30-60 pg/ml is considered optimal for increasing bone mass.
Some doctors prescribe a standard tablet dose such as 1 mg and then ask you how you are feeling the next time you come in. This is done for symptoms such as hot flashes, sleeplessness, depression, and so on, but is not helpful if you want help with osteoporosis where the symptoms are typically silent and revealed only upon having a DEXA scan or breaking a bone.
It can be difficult, but not impossible, to find a medical doctor who will prescribe estrogen, unless it’s only for short-term relief of post-menopausal symptoms. To use estrogen to prevent bone loss, you might have to find a functional, integrative, or naturopathic doctor. Also, if you are older and have been in menopause for some time, medical doctors don’t like to put you on it. It is unclear why.
Side Effects
It’s difficult to come up with a good list of side effects because the estrogen can be bioidentical or conjugated, and there are various modes of administration and strengths. In my opinion, bioidential hormone patches is the best way: lower doses and fewer, if any, side effects.
Second best, if cost is an issue, is bioidentical estrogen in tablet form. The drawback to the tablet is that you need a larger dose because it goes into your body through the gastrointestinal tract. Your body is made to absorb estrogen through skin tissue so transdermal estrogen is more efficient, works with a lower dose, and has fewer side effects.
Creams are transdermal too, but the estrogen doesn’t stay in your bloodstream as long. In my opinion, creams are fine for managing most menopause symptoms, but not for managing thinning bones.
A good natural supplement is DIM. DIM helps with estrogen metabolism (whether you still produce your own or are supplementing) and can help prevent hormone-related cancers. DIM is found in cruciferous vegetables, and is also available as a supplement, so you don’t have to eat 2 lbs of broccoli every day. See DIM for Hormone Balance and Vibrant Health.
References
Strontium
Strontium is a mineral that can increase bone density as it is measured by the DEXA scan. In the U.S. it is available as an over-the-counter dietary supplement.
- Strontium replaces calcium in the bone, but has a larger atomic weight. For every calcium atom replaced by strontium, the bone density appears larger, which artificially inflates the DEXA scan reading.
- Strontium is not naturally abundant in humans and does not have an identified, unique biological role.
- Strontium has potential safety risks and side effects that still need exploration.
The long-term effects of supplementing with strontium to increase DEXA scan results are not fully understood. It is not natural to bone in large amounts and might result in long-term problems, side-effects, and brittle bones. After you stop taking strontium, it can take a long time to leave your bone. For more information, see Smart Supplementing for Bone Health.
Strontium comes in several forms, as explained in this article: https://www.algaecal.com/algaecal-ingredients/strontium/. If you want to take strontium as a supplement, avoid strontium ranelate and make sure to take natural strontium salts (strontium citrate) instead. Strontium ranelate is a drug that is a synthetic form of strontium. People with kidney problems should not supplement with strontium, but should focus on foods that contain it instead. For a list of strontium food sources, see https://www.algaecal.com/algaecal-ingredients/strontium/strontium-rich-foods/.
Boron and Silica
Boron promotes bone building and resorption. It works best when taken in combination with other minerals so they can all work together to build strong bones. For a list of food sources, see https://www.algaecal.com/algaecal-ingredients/boron/boron-sources/.
Silica is an essential trace mineral for bone strength and density. It also strengthens skin, hair, and nails.
Chinese Herbs for Menopause Support
Chinese medicine recognizes the following herbs for managing menopausal symptoms: Wild yam, black cohosh, Dong Quai (aka Dang Gui, Tang Kuei, Dang Gwi, and Qin Gui).
And these herbs help to restore youthfulness: He Shou Wu (pure form) or Shou Wu Formulation (gentler).
Exercise
Exercise is important to maintaining bone health. It places mechanical stress on the bones, which stimulates bone remodeling. See Bone Remodeling and Bone Drugs. The type of exercise you get needs to be weight bearing, but it can be low impact, high impact, or both. Qi Gong, Tai Chi, and Yoga described below are all weight bearing and low impact forms of exercise. For more information, see https://www.americansportandfitness.com/blogs/fitness-blog/high-impact-vs-low-impact-exercises and weight bearing activities.
Yoga
Over 80% of the people in the study reversed their bone loss and began to gain bone. No fractures or serious injuries of any kind were seen or reported in over 100,000 hours of people doing this yoga daily. Over 80% of them had osteoporosis or osteopenia when we started. Fewer had these conditions when we finished.”
– Yoga for Osteoporosis article by Dr. Fishman, in Art of Living, August 3, 2020
- View Loren Fishman Sequence 1: Twelve Poses vs. Osteoporosis on YouTube for free.
- Purchase Dr. Fishman DVD(s) with sequence 1 and/or 2 on his website (sciatica.org) near the bottom of the page. Sequence 3 is out, but there is no DVD yet. On the same page at the bottom, you can sign up for his newsletter to find out when he teaches sequences 1, 2, and 3 online.
- The following books have helpful information regarding how to use yoga to improve your bone health:
- See Yoga Sequences for Bone Health for a list of poses in the sequences referenced above.
Does Yoga Really Work?
Sequences 1-3 are listed at the bottom of this page. You can scroll to the bottom and then back up to see them.
Dr. Fishman Sequence 1 has been proven to work for building bone density. It works particularly well for spine and femur necks. Dr. Fishman Sequence 2 is proving to be effective while it is currently under study. His Sequence 3 will be under study soon. The other bone health sequences in my collection make no claims one way or the other. See also An Interview with Loren Fishman and Ellen Saltonstall.
Non-Response
Some participants in the Dr. Fishman studies do not respond to the yoga sequences with better bone density. I asked him if the size and weight of the person makes any difference to how some people’s bones respond to the yoga sequence. I was figuring that larger, heavier people place more weight bearing stress on their bones in the poses. As of this writing (1/28/2021), Dr. Fishman responds to the question as follows: There appears to be a relationship between family history and non-response, but even that is not very secure at this point. There is no relation between size and response-rate at this point.
This made me wonder if muscle strength, rather than the size of the person, might be the key. Perhaps placing an emphasis on different kinds of weight-bearing exercise would add more bone-making to the body’s bone remodeling process. See Bone Remodeling and Bone Drugs.
In addition, proper nutrition, as described in this post, is key to building and maintaining bone density and bone health. In fact, upping my calcium intake by a lot was the key for me. For others it might be adding or upping another nutrient, or getting off of proton pump inhibitors (PPIs).
Repetitive Stress Syndrome
Doing the same poses every day in the same order can eventually result in pain from repetitive stress. To avoid this problem, consider doing something like the following as recommended by Dr Fishman:
- Dr. Fishman Sequence 1 once or twice a week, but not on consecutive days.
- Dr. Fishman Sequence 2 once or twice a week, but not on consecutive days.
- Dr. Fishman Sequence 3 once or twice a week, but not on consecutive days.
- Attend an Iyengar yoga class once or twice a week to learn how to do the poses correctly.
Liz Larson in Dr. Fishman’s office suggests an alternative where you make Sequence 1 the primary focus and add different poses from Sequences 2 and 3 over a week in addition to the 12 in Series 1. This way you work on different poses in Sequences 2 and 3 as add-ons to a Sequence 1 basic practice.
Dr. Fishman recommends practicing 4 days a week, but there is no harm in practicing every day or nearly every day. You could also substitute a Dr. Fishman sequence with one of the other sequences in Yoga Sequences for Bone Health towards the end of this post.
Physical therapy can be helpful as well. I saw a physical therapist for back pain. When he found out I also had osteoporosis, he added some exercises to help my bones. I’m sure those plus the yoga, plus the upped calcium intake all played a part in my adding a good amount of bone desnity on my last DEXA scan.
Hold Times and Technique
The DVDs and books specify hold times that you can use as a guideline. Think of the hold times as goals that you might eventually reach. The sequences listed at the end of this document do not specify hold times, but because that section is compiled from sources that do, you can follow the guidelines in the original sources or start out with 20 to 30 second holds and build up to 40 to 60 seconds, if possible.
Participants in Dr. Fishman’s yoga vs. osteoporosis dose-response study are advised to hold poses for a minimum of 12 seconds and a maximum of 72 seconds. Holding for 30 seconds is a good goal to work toward. Muscular strength needs to be built to reach the point where you can hold the pose long enough to strengthen the bone. When stress is placed on a bone, the chemical markers in blood that indicate bone building is occurring are evident beginning at the 12 second mark and stop at 72 seconds.
Forward Bends
Forward bends are not recommended for people with bone loss in their spine. Dr. Fishman says there have been studies showing that the vertebrae can crunch against each other and crack during forward bends.
However, forward bends are likely safe for experienced yoga practitioners who know how to keep their spines straight and their upper backs forward as they go down. Proceed at your own risk, and never force yourself to go further than is comfortable. Stop immediately if it hurts. See link to article under Twists.
Twists
Dr. Fishman sequences have twists. Many doctors will tell you not to do twists if you have osteoporosis. However, Dr. Fishman says that in all of his years working with osteoporosis, he has never encountered anyone who hurt themselves doing a twist. It’s up to you whether you do twists or skip them, but if you do want to twist, never twist to the point of strain. Never force a twist and stop immediately if it hurts For more information, see: https://yogauonline.com/twist-or-not-twist-dr-loren-fishman-weighs-safe-yoga-postures-for-osteoporosis-new-york-times (includes information about forward bends).
Qi Gong and Tai Chi
Qi Gong is a mind-body exercise that was developed in ancient China and Tibet. Qi Gong uses meditation, breathing, and movement to increase energy, stimulate the body’s healing abilities, and includes spiritual and healing benefits. Tai Chi is a gentle, self-paced system of gentle physical exercise and stretching.
Physical Therapy
Physical therapists can provide exercises that help build bone. You can find someone local to you, or if you prefer online, see Margaret Martin at https://melioguide.com/. She specializes in physical therapy for prevention and treatment of osteoporosis. She provides safe and effective exercise programs for strong bones, perfect posture, better balance, and core strength.
Yoga Sequences for Bone Health
This section presents 5 sequences for improving bone health. Dr. Fishman Sequence 1 is proven to work for building bone density. It works particularly well for spine and femur necks. Dr. Fishman Sequence 2 is proving to be effective while it is currently under study. Sequence 3 will be under study soon. The Patricia Walden and Baxter Bell sequences make no claims one way or the other.
For guidelines when doing these poses, see the following sections in this document: Repetitive Stress Syndrome, Hold Times and Technique, Forward Bends, and Twists.
Dr. Fishman Sequences 1-3
Sequence 1.
See Sequence 1: Twelve Poses vs. Osteoporosis on YouTube.
- Vrksasana
- Utthita Trikonasana
- Virabadrasana 2
- Utthita Parsvakonasana
- Parivrtta Trkonasana
- Salabasana
- Setu Bhandasana
- Supta Padangusthasana 1
- Supta Padangusthasana 2
- Marichyasana 3
- Ardha Matsyndrasana
- Savasana
- Tree
- Triangle
- Warrior 2
- Side Angle
- Revolved Triangle
- Locust
- Bridge
- Reclined Hand to Foot 1
- Reclined Hand to Foot 2
- Straight-legged Twist
- Ben Knee Twist
- Relaxation (corpse)
Sequence 2.
Purchase Dr. Fishman DVD(s) Sequence 1 or 2 on sciatica.org. Scroll to the bottom of the page.
- Tadasana
- Utkatasana
- Virabhadrasana 1
- Ardha Chandrasana
- Ustrasana
- Vasisthasana
- Dandasana
- Urdhva Muka Paschimottanasana
- Arm Threading (see CD)
- Bharadvajasana
- Jathara Parivartanasana
- Savasana
- Mountain
- Chair
- Warrior 1
- Half Moon
- Camel
- Side Plank
- Staff
- Upward Legs Stretch
- Similar to Eagle pose (see CD)
- Twist with legs to one side
- Supine Twist
- Relaxation (corpse)
Sequence 3.
No DVD available yet. Sign up for Dr. Fishman’s newsletter at sciatica.org (scroll to the bottom of the page) to get email notices for his classes including his Yoga for Osteoporosis sequences. You can purchase any class through the newsletter,
- Modified Parsvottanasana
- Natarajasana
- Rajakapotasana
- Virabhadrasana 3
- Parivrtta Ardha Chandrasana
- Parivrtta Parsvakonasana
- Ardha Purvottanasana or substitute Purvottanasana
- Khumbhakasana
- Supta Padangusthasana 1
- Supta Padangusthasana 2
- Gomukasana
- Savasana
- Intense side stress modified to 90 degree angle only.
- Dancing Pose
- One-Legged King Pigeon
- Warrior 3
- Revolved Half Moon
- Revolved Side Angle
- Reverse Table Top or substitute up plank
- Plank
- Reclined Hand to Foot 1
- Reclined Hand to Foot 2
- Cow Face Pose on floor
- Relaxation (corpse)
Baxter Bell Sequence for Bone Strength
This sequence is available in Yoga for Healthy Aging by Baxter Bell and Nina Zolotow and also available on their Yoga for Healthy Aging blog. To find it, go to Holiday Presents, Day 1!, scroll down to the PDF, and then scroll to page 44 in the PDF.
- Bitilasana-Marjaryasana
- Dandayamana Bharmanasana
- Adho Mulkha Svanasana
- Khumbhakasana
- Tadasana
- Virabhadrasana 1
- Utthita Parsvakonasana
- Utkatasana
- Virabhadrasana 3
- Adho Mukha Svanasana
- Khumbhakasana
- Balasana
- Salabhasana
- Marichyasana 3
- Setu Bhandasana
- Savasana
- Dynamic Cat-Cow
- Hunting Dog
- Downward Dog
- Upwards Plank
- Mountain
- Warrior 1
- Extended Side Angle
- Powerful (Chair) Pose
- Warrior 3
- Down Dog (use foreamrs instead of hands)
- Plan from Knees (instead of toes)
- Child’s Pose
- Locust
- Sage’s Twist
- Bridge Pose
- Relaxation (corpse)
Patricia Walden Sequence
Important: Forward bends are not recommended for people with bone loss in their spine. If forward bends are a problem for you, you can skip them, modify the poses so that you keep a straight back with your chest forward, or substitute another pose. For more information, See Forward Bends in this document.
This sequence has the following forward bends:
- Uttanasana
- Parsvottanasana
- Prasarita Padottanasana
- Standing forward bend
- Intense side stretch
- Wide-angled forward bend
- Substitute Dandasana
- Bend to a 90 degree angle
- Bend to a 90 degree angle
This bone health sequence is available in the book Yoga for Healthy Bones by Linda Sparrowe. It is also available at A Sequence for Preventing/Reversing Bone Loss on the Yoga for Healthy Aging blog. See also Patricia Walden’s website for class information.











































































 The extent of the climate change in the Arctic Polar region is far more significant than reported in the general news. Richard Engel (NBC and MSNBC) reported that he was in Iceland 5 days ago and he stood on the very last remaining glacier in all of Iceland. It was melting so quickly that Engel thinks it too will be gone sometime next year. Iceland may need to change its name!
The extent of the climate change in the Arctic Polar region is far more significant than reported in the general news. Richard Engel (NBC and MSNBC) reported that he was in Iceland 5 days ago and he stood on the very last remaining glacier in all of Iceland. It was melting so quickly that Engel thinks it too will be gone sometime next year. Iceland may need to change its name!



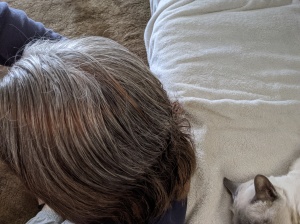
 He recommended which products to start with given our description of what Ollie was going through. After that, it took some experimentation to find exactly the right combination of products, the right dosages, and the right way to administer them — in their food or with a syringe.
He recommended which products to start with given our description of what Ollie was going through. After that, it took some experimentation to find exactly the right combination of products, the right dosages, and the right way to administer them — in their food or with a syringe. It became clear right away that using a syringe was not going to work with Ollie. He fought it tooth and nail and we knew the added stress was not doing him (or me) any good. So, we tried putting the supplements in their wet food. We started with
It became clear right away that using a syringe was not going to work with Ollie. He fought it tooth and nail and we knew the added stress was not doing him (or me) any good. So, we tried putting the supplements in their wet food. We started with 


 After washing my hair a couple of times over the next week, it is easier to see how my hair is starting to turn brown (see photo at left). At this point it still has some burgundy highlighting, which you can see in the middle of the photo.
After washing my hair a couple of times over the next week, it is easier to see how my hair is starting to turn brown (see photo at left). At this point it still has some burgundy highlighting, which you can see in the middle of the photo.



 Looking underneath you can see that the hair is getting darker with the henna to indigo ratio changing. Light coming in through a window makes the henna red seem stronger than it actually is.
Looking underneath you can see that the hair is getting darker with the henna to indigo ratio changing. Light coming in through a window makes the henna red seem stronger than it actually is.